About COVID-19
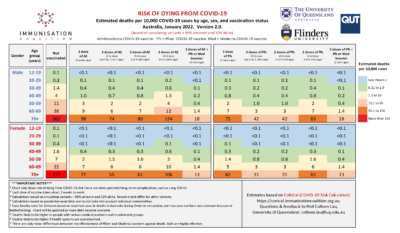
COVID-19 Risk Chart
The Immunisation Coalition in collaboration with the University of Queensland, QUT and Flinders University have developed a COVID-19 Risk Chart which shows the estimated COVID-19 deaths per 10,000 cases by age, sex, and vaccination status in Australia as at January 2022.
This chart is a useful tool for Healthcare practitioners and the public to help assess the risks associated with COVID-19 for the unvaccinated as well as the those who have received vaccines.
Click on the icon below to view or download the chart:
What is COVID-19?
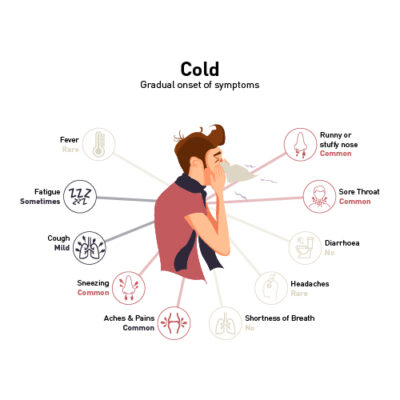
COVID-19 is a disease caused by a new form of coronavirus, first reported in December 2019. Coronaviruses are a large family of viruses that cause respiratory infections. These can range from the common cold to more serious diseases.
Watch the video on the WHO website
Variants
Covid 19 viruses can mutate (change) themselves when they replicate (make copies of themselves). Viruses that have mutated in this way are called variants.
COVID 19 variants that have caused past waves of infection are alpha and delta and belong to the Covid 19 family tree. The omicron variant emerged in late 2021 and it has mutated into an abundance of subvariants. This swarm of variants has been referred to as a” variant soup”. In Australia the most common sublineages that have emerged from Omicron are: BA.2, BA.5, BA.4, BQ.1 and XBB.
Some variants may be more contagious, may evade immunity (making vaccines and treatments less effective), may be more severe (causing more hospitalisations and deaths) and they may be harder to detect with Rapid Antigen Tests (RATs).
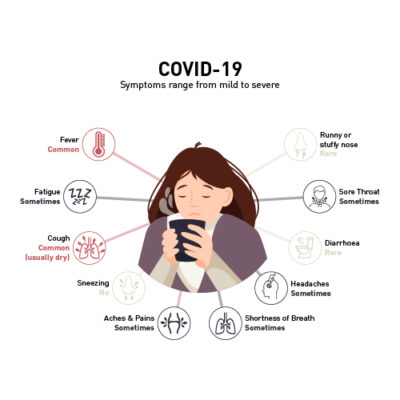
COVID-19 Symptoms
Symptoms of COVID-19 can range from mild illness to pneumonia. Most people will recover easily, and others may get very sick very quickly. People with coronavirus may experience symptoms such as:
- fever
- respiratory symptoms which may include a sore throat, coughing, runny or blocked nose
- shortness of breath
Other symptoms can include headache, muscle or joint pains, nausea, diarrhoea, vomiting, loss of sense of smell, altered sense of taste, loss of appetite and fatigue.
 If you are concerned that you, or anyone close to you may have COVID-19 symptoms, you can use the HealthDirect COVID- 19 Symptom and Antiviral Eligibility Checker and go to a testing centre near you.
If you are concerned that you, or anyone close to you may have COVID-19 symptoms, you can use the HealthDirect COVID- 19 Symptom and Antiviral Eligibility Checker and go to a testing centre near you.
How COVID-19 Spreads
The virus can spread from person to person through:
- close contact with an infectious person (including in the 48 hours before they had symptoms)
- contact with droplets from an infected person’s cough or sneeze
- touching objects or surfaces (like doorknobs or tables) that have droplets from an infected person, and then touching your mouth or face.
Current evidence suggests that the most likely spread is from respiratory droplets between people from close contact with each other.
People are believed to be most infectious two days before they start showing symptoms. However even if people do not show any symptoms, they can still spread the virus to other people.
Watch the video on the WHO website.
COVID-19 Complications
Most people will recover from Covid 19 within a few weeks however 1 in 6 may experience complications. Older people and those with underlying medical conditions e.g., heart disease or diabetes may be more likely to develop a more serious illness.
What causes Covid 19 complications?
Covid 19 complications may be caused by a cytokine storm. Cytokines are inflammatory proteins that can flood the bloodstream after an infection like COVID 19 triggers the immune system. The large influx of cytokines can cause damage to many organs of the body like the heart, lungs, liver and kidneys.
The most common complications are of the lungs and respiratory system, they are:
- Acute Respiratory Failure: a serious condition when the lungs can’t get enough oxygen to the rest of the body and there is a build-up of carbon dioxide causing damage to other organs of the body
- Pneumonia: an infection that affects one or both lungs. The air sacs in the lungs become inflamed making it harder to breathe. This type of pneumonia may cause scar tissue and long-term damage to the lungs
- Acute Respiratory Distress Syndrome: the lungs become so severely damaged that fluid flows into them which inhibits the body getting oxygen into the bloodstream
The other complications may be:
- Acute liver injury: when the liver suddenly stops working
- Acute cardiac injury: damage to the heart
- Secondary infection: when the body develops another infection unrelated to Covid-19 e.g., a bacterial infection like Strep or Staph
- Acute kidney injury: an abrupt decrease in kidney function
- Septic shock: a life-threatening condition when the blood pressure drops to a dangerously low level after an infection
- Disseminated intravascular coagulation: the body doesn’t clot properly, forming abnormal clots which can lead to internal bleeding and organ failure
- Blood clots: clumping of blood cells in the blood vessels
- Multisystem inflammatory syndrome in children: some organs in the body become severely inflamed. Symptoms include fever, belly pain, vomiting, diarrhoea, headache, rash and confusion
- Chronic fatigue: Symptoms may include brain fog, severe fatigue, pain, trouble thinking or dizziness
- Rhabdomyolysis: muscles break down and tissues die. As the cells break, a protein is released into the bloodstream which if the kidneys can’t clear, it could be fatal
- Damage to the brain: Even in young people, COVID-19 can cause strokes and Guillain barre syndrome which is a condition where the immune system attacks the nerves and can cause paralysis. COVID-19 may also increase the risk of Parkinson’s disease and Alzheimer’s disease
- Dermatologic: Rash
- Neurologic: Loss of taste, smell and sleep disturbance
- Psychiatric: depression, anxiety, changes in mood
People with severe symptoms may be hospitalised and treated in the Intensive Care Unit with mechanical devices such as ventilators. Surviving these experiences can make them more likely to suffer from post traumatic stress disorder, depression and anxiety.
COVID-19 Prevention
There are several things you can do to prevent the spread of COVID-19, such as;
- Practise good hygiene, wash your hands, keep home and workplaces clean and covering your mouth when you cough
- Social Distancing, keeping at least 1.5 metres away from other people in the home and public areas even if they are not showing symptoms
- Masks: wear masks if you are in an area where physical distancing is not possible. Make sure the mask covers your nose and your mouth
- Quarantine, if travelling to other countries you may be required to isolate or quarantine upon arrival. People travelling to Australia from China may be required to show evidence of a negative pre-departure test for COVID-19. Quarantine and testing requirement when travelling may change at any time. Check here for the current recommendations.
- Isolate, if you have contracted COVID-19 it is strongly recommended that you stay at home. Although it is no longer a legal requirement to isolate, staying at home protects the people around you and the general community from COVID-19. You should avoid entering high risk settings like aged and disability care facilities and hospitals unless seeking immediate medical care. At home, keep the room well ventilated. Monitor yourself for any symptoms and call your health care provider if you have difficulty breathing, loss of speech or mobility, confusion or chest pain. Stay positive, contact family and friends regularly, maintain regular exercise at home and monitor your mental health. The isolation period is 7 days or when symptoms have resolved, whichever is the longer period.
- Vaccine, Australia’s vaccination of it’s population against COVID-19 is well under way, you can read more about the vaccination program here
- Vaccine boosters, are recommended by the Australian Technical Advisory Group on Immunisation (ATAGI). Read the recommendations here.
Do you have questions about getting vaccinated against COVID-19? Dr Margie Danchin, from @UniMelbMDHS and leader of Vaccine Acceptance, Uptake and Policy at @MCRI_for_kids answers some key questions being asked by the Australian community about COVID-19 vaccines. pic.twitter.com/Ecr7pj4CSj
— University of Melbourne (@UniMelb) July 23, 2021
For more information on how these vaccines work see The Different Types of COVID-19 Vaccines article from the WHO.
Watch video on WHO website
Pre-exposure prevention
Evusheld (tixagevimab and cilgavimab) received provisional approval on 24 February 2022 for the pre-exposure prevention of COVID-19 in adults and adolescents aged 12 years and older. For people who are immunocompromised or who have a history of a severe adverse reaction to the COVID-19 vaccine, Evusheld may be considered.
Tixagevimab and cilgavimab are monoclonal antibodies that stick to the spike protein on the COVID 19 virus and stop it from getting into your lungs.
COVID-19 Treatment
Doctors will need to review patients’ medications and their current medical conditions to decide if a COVID-19 treatment is suitable for them. The types of COVID-19 treatments that are suitable will also depend on the severity of their COVID-19 illness.
Basic in hospital treatment options include: oxygen for severely ill patients, ventilation for patients who are critically ill and the use of Dexamethasone or other corticosteroids. Antivirals, immune modulators and monoclonal antibodies have also been used.
Severity of COVID-19
Mild Illness: Individuals who have any of the various signs and symptoms of COVID-19 (e.g., fever, cough, sore throat, feeling unwell, headache, muscle pain, nausea, vomiting, diarrhea, loss of taste and smell) but who do not have shortness of breath, difficulty breathing or abnormal chest imaging. These individuals do not require oxygen.
Moderate Illness: Individuals who show evidence of lower respiratory disease (e.g. pneumonia) during clinical assessment or imaging and who have low oxygen levels. These individuals require oxygen.
Severe Illness: Individuals who have lower respiratory disease with severely low levels of oxygen in their blood. These individuals require oxygen.
Critical Illness: Individuals who have respiratory failure (where the lungs have trouble loading oxygen or removing carbon dioxide), septic shock (blood pressure drops to a dangerously low level after an infection), and/or multiple organ dysfunction. These individuals require oxygen.
COVID-19 Treatments
| Drug | Mild COVID-19 Severity (Not requiring oxygen) | Moderate COVID-19 Severity (Requiring oxygen) | Severe COVID-19 Severity (Requiring oxygen) | Critical COVID-19 Severity (Requiring oxygen) |
|---|---|---|---|---|
| Dexamethasone | X | ✓ | ✓ | ✓ |
| Veklury (remdesivir) | X | ✓ | ✓ | ✓ |
| Xevudy (sotrovimab) | ✓ | X | X | X |
| Ronapreve (casirivimab + imdevimab) | ✓ | X | X | X |
| Paxlovid (nirmatrelivir + ritonavir) | ✓ | X | X | X |
| Lagevrio (molnupiravir) | ✓ | X | X | X |
| Baricitinib | X | ✓ | ✓ | ✓ |
| Tocilizumab | X | X | ✓ | ✓ |
Mild COVID-19 Severity
The medications currently available for mild disease are:
Monoclonal antibodies
Xevudy (sotrovimab)
The TGA provisionally approved Xevudy® on 20 August 2021. Xevudy can be used within the first 5 days of symptoms starting in patients aged 12 years or older with mild to moderate COVID-19 who are at high risk of progression to severe disease.
Xevudy (sotrovimab) is a monoclonal antibody which sticks to the spike protein on the COVID-19 virus. This stops the virus getting into the lungs and causing an infection.
Ronapreve (casirivimab + imdevimab)
Ronapreve has also been provisionally approved for the treatment of COVID-19 in adults and adolescents (aged 12 and older) who do not require the initiation of oxygen and who are at increased risk of progressing to severe disease.
Casirivimab and imdevimab are monoclonal antibodies that also stick to the spike protein of the COVID-19 virus and stop it from getting into the lungs.
Antivirals
The TGA provisionally approved the first oral treatments for COVID-19 in Australia, molnupiravir (Lagevrio®) and nirmatrelvir + ritonavir (Paxlovid®), on 18 January 2022. They both have provisional approval for the treatment of adults with COVID-19 who do not require initiation of oxygen due to COVID-19 and who are at increased risk of hospitalisation or death.
Paxlovid (nirmatrelivir + ritonavir)
Nirmatrelvir is a protease inhibitor that treats COVID-19 by blocking a certain protease, a protein the virus needs to make copies of itself and continue to infect. Ritonavir is also a protease inhibitor. Low-dose ritonavir is included in Paxlovid to slow the breakdown of nirmatrelvir, allowing it to stay in the body longer to fight COVID-19.
Lagevrio (molnupiravir)
Molnupiravir is a nucleoside analogue, which means it mimics some of the building blocks of RNA. Molnupiravir gets incorporated into the RNA of the COVID-19 virus and causes havoc so that the virus dies as it cannot replicate itself.
PBS eligibility criteria for Lagevrio and Paxlovid (1st November 2022)
If you test positive for COVID-19, you may be eligible for antiviral treatments if you are:
- 70 years of age or older, regardless of risk factors and with or without symptoms
- 50 years of age or older with 2 additional risk factors
- First Nations person, 30 years of age or older and with 1 additional risk factor
- 18 years of age or older and moderately to severely immunocompromised.
Check your risk factors and eligibility here.
Moderate, Severe and Critical COVID-19 Severity
Corticosteroids
Dexamethasone or other corticosteroids can be considered for patients who require oxygen during the inflammatory phase of illness. Corticosteroids reduce inflammation. The RECOVERY trial showed a benefit with corticosteroids at reducing deaths only during the inflammatory phase of the illness.
Antivirals
Veklury (remdesivir)
The Therapeutic Goods Administration (TGA) provisionally approved Veklury® on 10 July 2020. Veklury can be used in adults hospitalised with moderate to severe COVID-19.
Veklury works by interrupting production of the COVID 19 virus. It interferes with one of the key enzymes the virus needs to replicate RNA. This prevents the virus from multiplying.
Veklury (remdesivir) was shown to shorten the time to recovery in adults who were hospitalised with COVID-19.
Immune Modulator
Olumiant (baricitinib), an immune modulator has been used off-label for patients with COVID-19 who require oxygen.
Monoclonal Antibody
RoActemra (tocilizumab), a monoclonal antibody, has been used off-label with dexamethasone in patients with COVID-19 receiving oxygen and having evidence of systemic inflammation.
In the USA and Europe, baricitinib, and tocilizumab have been recommended for use with or without dexamethasone and/or remdesivir.
Treatments lacking evidence to support their use in people with COVID 19
Ivermectin, doxycycline and zinc
There is currently insufficient evidence to support the safe and effective use of ivermectin, doxycycline and zinc (either separately, or in combination) for the prevention or treatment of COVID-19.
Hydroxychloroquine
The use of hydroxychloroquine (with or without zinc) for the treatment of COVID-19 is not recommended by regulators or the WHO as there is concern that, if used inappropriately, may cause toxicity and lead to adverse patient outcomes.
Hydroxychloroquine has well known risks including cardiac toxicity, irreversible eye damage, and severe depletion of blood sugar levels (which could lead to coma).
Natural Treatments
Natural treatments such as zinc, melatonin, vitamin C, vitamin D, and other supplements are readily available and commonly used to help prevent or treat COVID-19; however, there is insufficient data to recommend the use of such for the prevention or treatment of COVID-19.
The Immunisation Coalition takes an evidence-based approach to COVID-19 treatment.
- World Health Organization. Coronavirus disease (COVID 19). Overview. 2022 https://www.who.int/health-topics/coronavirus#tab=tab_1
- Australian Government Department of Health and Aged Care. COVID-19 disease and symptoms Last updated 14 October 2022
- World Health Organization. Coronavirus disease (COVID-19): How is it transmitted? Accessed 19 October 2022
- Brooks JT, Butler JC. Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2. JAMA. 2021;325(10):998–999. doi:10.1001/jama.2021.1505
- Callaway E. COVID ‘variant soup’ is making winter surges hard to predict. 2022 Oct 28. https://www.nature.com/articles/d41586-022-03445-6
- Post-COVID conditions: Information for healthcare providers. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html. Accessed 4 Jul 2021
- Post-COVID-19 conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects.html. Accessed 4 Jul 2021
- COVID-19 (coronavirus): Long-term effects, Mayo Clinic, https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-long-term-effects/art-20490351. Accessed 4 July 2021
- National COVID-19 Clinical evidence Taskforce: Australian Guidelines for the clinical care of people with COVID 19 version 53.1 Published 08 March 2022
- Australian Government Department of Health: Medications for People with COVID-19 Reviewed 11 March 2022
- Australian Government Department of Health; COVID-19 Treatments 04 March 2022
- Australian Government Department of Health Oral treatments for people with COVID-19 Last updated 03 November 2022
- Australian Government Department of Health TGA Product Information Evusheld Date of first Approval 26 February 2022. Last updated 23 September 2022
- Australian Government Department of Health TGA Product Information Ronapreve Date of Revision 10 December 2021
- Australian Government Department of Health TGA Product Information Paxlovid Date of first Approval 20 January 2022
- Australian Government Department of Health Updated eligibility for oral COVID-19 treatments last updated 1 November 2022
More COVID-19 Information
Australian Department of Health: Coronavirus (COVID-19) resources for the general public
ACT Government: COVID-19
Department of Health and Human Services Victoria: Coronavirus (COVID-19)
Coronavirus Victoria: Translated information about COVID-19
Coronavirus Victoria: Symptoms and Risks
Coronavirus Victoria: Education – Information for parents, students and educators
NSW Health: COVID-19 Frequently Asked Questions
Northern Territory Department of Health: Coronavirus
Western Australia: COVID-19 (Coronavirus)
Queensland Health: Coronavirus(COVID-19)